What is and how to treat panic attack/panic disorder using supportive psychotherapy
History of panic disorder
- Anxiety Disorders and panic attacks were often thought a women's problem.
- Since Adam and eve humans have experienced panic attacks. Like the forbidden fruit, stimulus is what drives our survival mechanism which triggers the fight, flight or freeze response which stimulate the stress hormone Epinephrine (adrenalin)
- In the medieval/ancient times treatments were various from herbs, bathing in extremely cold rivers , streams, health spas, and blood letting using leeches
- Freud's concept in 1895 of anxiety neurosis was used as a major organizing principle which was related compatible with panic disorder and agoraphobia (fear of stimulus) . This was commonly diagnosed when no natural cause could be found for vague physical complaints.
- Panic/Anxiety disorders were only recognized by American Psychiatric Association as a psychiatric condition in 1980
- Until then people experiencing these disorders usually received a generic diagnosis of stress or nervousness.
- Panic disorders is known as a maladaptive response to (fear and anxiety) as excessive arousal presents itself even after a threat is no longer present (survival mech malfunction).
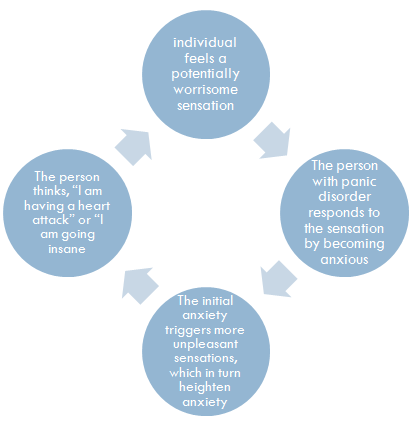
Panic disorder cycle
Symptoms
Panic attacks follow four of the following symptoms
- short bouts of panic that reach peak within 10 min
- Palpitations of the heart
- Tingling in the hands or feet
- Shortness of breath
- Sweating
- Hot and cold flashes
- Trembling
- Chest pains
- Chocking sensation
- Faintness
- Dizziness
- And a feeling of unreality
- Panic attacks are onsets to panic disorder
Symptoms of panic disorder
- Panic attacks that are recurring last 10-20. However are unexpected and without apparent reason.
- Dysfunctional change in thinking or behavior as result of attacks
- Worry persistently about having additional attacks
- Plan their lives around the possibility of future attacks fear loss of control
- Agoraphobia – afraid to leave the house to public places where escape might be difficult or help unavailable should panic symptoms develop
Incidence & Prevalence
- More then one-quarter of the population have one or more panic attacks at some point.Around 2.8% of
- united states suffer from panic disorder each year; close to 5% develop one of patterns some point in their
- Panic disorder tends to develop in late adolescence or early adulthood
- Woman are twice as likely to be diagnosed with panic disorder
- Panic disorder is the same across various cultural and racial groups in the united states
- Surveys indicate that around 35% of individuals with panic disorder in the united states are currently in treatment
- Similarly the disorder occur in equal numbers in cultures across the world although specific content differs from country to country
Causes
Biological cause
- Circuits that produce panic reaction are areas in amygdala, hypothalamus, central gray matter and locus ceruleus
- Hyperactive Amygdala increases symptom severity as it processes emotional information (fight or flight) and is an important neural circuiting of fear and anxiety
- Hypothalamus irregularity occurs later in the course of the disorder, after the development of anticipatory anxiety and associated stress
- panic attacks are mediated at midbrain dorsal called the periaqueductal (gray matter) this controls pain and analgesia (extreme pain without loss of conscious), fear and anxiety, vocalization, lordosis (forward curvature of the spinal column) and cardiovascular control.
- Epinephrine irregularity is linked to panic disorder and depression
- Locus ceruleus which (regulates emotions) becomes rich with epinephrine.
- Genetic to play a roll. fraternal twins 11 % share the same disorder, while 31% with identical twins (share all genes)
cognitive cause
- Panic prone have a higher degree of anxiety sensitivity which they force on bodily sensations much of the time and are enable to assess them logically
- As Panic prone the individuals hone in on particular bodily sensations, and misinterpreting them as signs of medical catastrophe.
- The panic-prone grow increasingly upset about losing control, fearing the worst, they lose all perspective and rapidly plunge into panic.
- over breathing/hyperventilation abnormal breathing that makes individuals believe they are in danger of suffocation
- Individuals develop beliefs that dangerous sensations may return, setting themselves up for future panic attacks.
- there are also connections associated with major life changes.
Case study
History of Mr. J
- 50-year-old married man who had no previous history of psychiatric disorders
- he had no medical hospitalizations, no chronic medical problems
- was a successful businessman who owned a corporation (high functioning)
- worked approximately 60 hours per week
- Main complaint was “I had a car accident”
- vehicle pulled out in front of him and did not yield despite Mr. J's right of way.(no one was injured)
- The driver of the other vehicle was an elderly man, and his wife was a passenger
- following the accident he was referred to the emergency department the only abnormality elevated blood pressure. after accident Developed hypertension (no psychical cause)
- To treat Hypertension he was started on meds amlodipine (Treats high blood pressure)
- a second antihypertensive metoprolol was added (given after a heart attack to improve outcomes)
- He was suggested a third antihypertensive causing the client increased anxiety and feelings of being (out of control). He was then referred to psychiatric consultation at that point.
Symptoms of Mr. J
- He experienced primary symptoms depersonalization(loss of control), palpitations, chest pressure, shortness of breath, and tremulousness
- The anxiety reportedly occurred several times daily, lasted for 15-20 minutes.
- He avoided driving due to his fear of experiencing an anxiety attack rather than fear of another motor vehicle accident(Agoraphobia).
Treatment
supportive psychotherapy (Involves psychodynamic , cognitive behavior)
(Higher functioning individual)
- Supportive psychotherapy educates client in treatment. The client is guided though the body's (fight or flight) response learning to recognize and identify sensations (important initial step toward treatment of panic disorder)
- The goals of supportive psychotherapy is to strengthen coping skills to reducing behavioral dysfunction and mental distress while reinforcing the clients healthy and adaptive patterns of thought behaviors
- This enables the clients to readapt using already developed personal resources rather then becoming inappropriately dependent on psychiatrist
Cognitive / behavioral
- cognition that occurred during and after accidents (clients will not do this, fear of re-experiencing the trauma)
- therapist explains cognition during recount provides information for irrational belief presence (fears of dyeing) and develop rational alternative thoughts
- as with phobias exposure treatments such as desensitization allows client to build hierarchy of fears in which they may gradually confront.
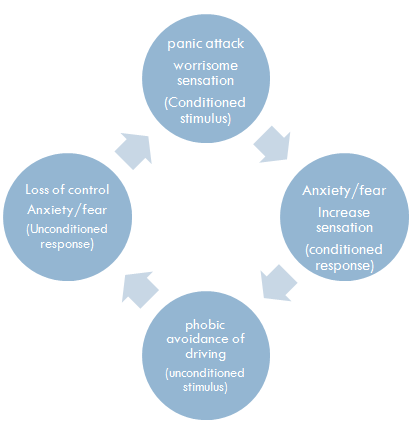
Cognitive/ behavioral diagnosis
- Panic attacks accompanied by phobic avoidance of driving were among the main sources of anxiety
- During the first session, the client himself was able to realize that not driving was resulting to his psychological and social problems.
- The client also spontaneously engaged in behavioral strategies helpful in managing depression and anxiety. (yoga, treadmill exercises and meditation)
- Panic attack with Agoraphobia - avoidance of driving was the diagnosis
- Exposure treatment such as desensitization would be used, and a hierarchy of fears would be introduced. in this case side streets, freeways, city interchanges, rush hours, developing a gradual plan of exposure. (“behavioral” reduces anxiety associated with having a panic attack)
agoraphobia cycle
supportive psychotherapy Diagnosis
supportive psychotherapy for Mr. J (Involves psychodynamic , cognitive behavior)
- Mr. J stated he felt “abandoned” by his mother since age of five years, (marital difficulties) he was raised by grandparents
- Mr. J was angry that the elderly couple (other drivers) had not apologized nor attempted any contact.
- his mother, suffered from multiple medical problems, including Alzheimer's disease and hypertension before her death.
- Mr. J attempted to reconnect with his mother however due to her state he was unable to achieve closure
- the elderly denied Mr. J compassion and acknowledgment of his emotional and physical pain likely caused the resurfacing of unresolved issues making him more vulnerable to psychiatric pathology, such as new onset panic disorder.
- The clients had unmet dependency needs in the past and, therefore, the potential for hostility when these needs were not acknowledged now.
- He was given alprazolam (xanax) and after 8 weeks discontinued use. His blood pressure normalized as the anxiety symptoms subsided.
- Stimulus his mother's previous medication regimen
- So, is Dependency onset to panic attacks?
Panic cycle
prevention
- Panic prone individuals should avoid stressful situations
- Avoid becoming to dependent
Work cited
- Jeyce Willig Quintino-dos-Santos, Cláudia Janaína Torres Müller, Cristie Setúbal Bernabé, Caroline Azevedo Rosa, Sérgio Tufik, Luiz Carlos Schenberg " Evidence That the Periaqueductal Gray Matter Mediates the Facilitation of Panic-Like Reactions in Neonatally-Isolated Adult Rats" US National Library of Medicine National Institutes of Health; journal list, published online 2014 Mar 3
- Jieun E Kim, Stephen R Dager, In Kyoon Lyoo "The role of the amygdala in the pathophysiology of panic disorder: evidence from neuroimaging studies" US National Library of Medicine National Institutes of Health; journal list, published online 2012 Nov 20
- Behbehani MM "Functional characteristics of the midbrain periaqueductal gray" US National Library of Medicine National Institutes of Health; journal list, published online 19195 Aug
- Natasha Tracy, History of Anxiety Disorders. Healthyplace. web. 02 October 2008, updated 14 January 2014
- John M. Grohol. National Institute of Mental Health, Treatment of Panic Disorder. Web. 30 Jan 2013.
- Julie P. Gentile MD, Ann Morrison MD "A Man Develops Panic Disorder After a Car Accident" US National Library of Medicine National Institutes of Health; journal list, published online 2004 Nov
- Comer j. ronald. New York, worth publishers. Fundamentals of abnormal psychology 2005,2008,2011.
- Frances A, Miele GM, Widiger TA, Pincus HA, Manning D, Davis WW. " The classification of panic disorders: from Freud to DSM-IV" US National Library of Medicine National Institutes of Health; journal list, published online 1993